Post-herpetic Neuralgia: Symptoms And Causes
Post-herpetic neuralgia is the most common complication of shingles. This relatively common viral infection in the general population does not always evolve with this consequence, but when it does, it creates a major problem.
What usually happens is that a person is infected with the herpes zoster virus or chickenpox. This infection can go unnoticed, it can manifest itself with the symptoms of chickenpox –especially in children- or it can be expressed with what is known as ‘shingles ‘ .
Shingles is the first herpes zoster infection in an organism. Lesions appear as small blisters on the skin following the path of the nerve where the virus is housed. The most common locations are the ophthalmic nerve, the trigeminal nerve in the face, and some intercostal nerves in the chest.
These blisters are accompanied by severe pain, such as burning. After about a month, the skin lesions disappear and little by little the pain of this first infection subsides.
The underlying problem is that the virus is still lodged in the nerve, although it does not manifest itself. Later, some people experience very severe pain in the same region where they had the first infection, but this time without skin lesions. That’s postherpetic neuralgia.
Older people are more likely to suffer from it, especially those over sixty years of age. While there is no curative treatment, steps can be taken to alleviate symptoms.
Causes of postherpetic neuralgia
The origin of postherpetic neuralgia is clear: it is the herpes zoster virus. The main characteristic of this microorganism is that it remains lodged in the nerves of the human being for life, although it does not manifest itself with symptoms.
When the person who has the virus inside them ages or their immune system decreases its activity, then it reactivates. Reactivation can be expressed as postherpetic neuralgia, that is, severe pain in the affected nerve.
The pain is very intense and with a burning sensation because the infected nerve is damaged. The virus causes destruction of some nerve fibers that transmit information. With the fibers destroyed, the nerve information is confusing to the brain, which interprets it as pain.
Beyond the main cause of the disease, there are risk factors that make its appearance more likely. These are:
- Age: over sixty years the frequency increases.
- Characteristics of the initial infection: If the first appearance of herpes zoster was severe, there is an increased risk of later neuralgia.
- Chronic diseases: people with diabetes, for example, are at higher risk.
- Location: the face and, particularly, the ophthalmic area are more painful.

Symptoms of the disease
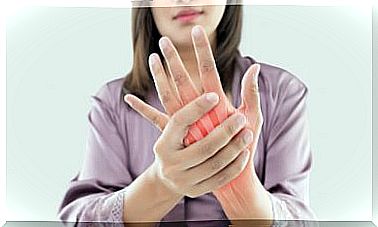
The symptom of postherpetic neuralgia is pain. It appears in a certain area that corresponds to the infected nerve. Normally, it is an area that months or years before was affected by the blisters from the first infection.
If left to evolve on its own, in most cases the pain would last six months. But in some people, without treatment, it can become indefinite pain. There are cases that can be considered as disabling pain.
We could say that the three basic symptoms of the disease are:
- Pain: intense, burning, with a particular path and easily identifiable by the patient; with a persistence of months.
- Sensitivity: in the affected area, even contact with clothing stimulates and triggers pain.
- Itching: the affected nerve sends confusing signals to the brain, which are interpreted as an itch in the affected territory.

Treatment of postherpetic neuralgia
There is no cure for the disease. The virus will remain lodged in the nerve throughout the life of the person who has it. However, there are therapeutic alternatives for treating pain and improving quality of life.
The first step in treatment is common non-steroidal anti-inflammatory drugs. Although in many countries they are available over the counter, they should be prescribed by a professional, due to their possible adverse effects. The most commonly used anti-inflammatories for postherpetic neuralgia are ibuprofen and naproxen. But people with high blood pressure, gastritis or anticoagulants cannot take them freely without supervision.
The second step of treatment is other pain relievers. The simplest is paracetamol, although the intensity of the pain can even lead to the use of narcotics. In this case, obviously, only with a medical prescription.
They are experimenting with botulinum toxin, seeking treatment alternatives. The first reference to the use of this treatment is relatively recent, from the year 2002. More studies are required, but the expectation is promising. The other two medications that are not specifically pain relievers, but that have been proven effective are anticonvulsants and tricyclic antidepressants.
As a disease with a complex approach, it does require professional intervention. If you suffer from pain suspected of postherpetic neuralgia, a medical consultation is essential. The health team will know how to guide you with the relief measures and with the type of medications that you can consume.